-Excretion and Osmoregulation
Maharashtra Board-Class-11-Science-Biology-Chapter-15
Notes-Part-2
Topics to be Learn : Part-2
|
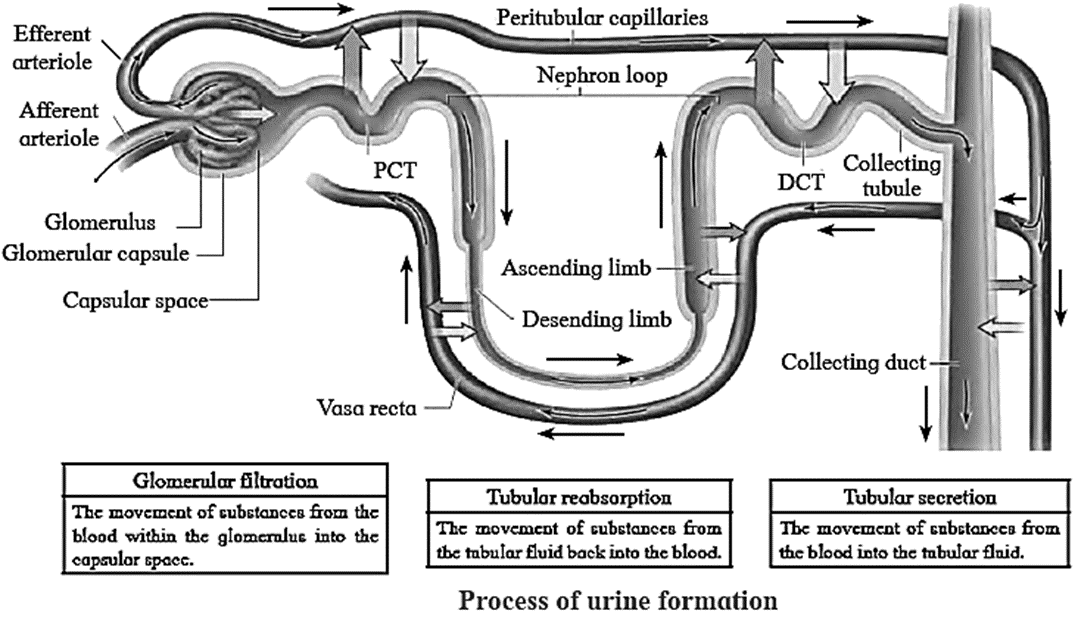
Urine Formation
Process of urine formation is completed in three successive steps as-
- Ultrafiltration / Glomerular filtration,
- Selective reabsorption,
- Tubular secretion / Augmentation.
Ultrafiltration / Glomerular filtration :
- Diameter of afferent arteriole is greater than the efferent arteriole. The diameter of capillaries is still smaller than both arterioles. Due to the difference in diameter, blood flows with greater pressure through the glomerulus. This is called as glomerular hydrostatic pressure (GHP) and normally, it is about 55 mmHg.
- GHP is opposed by osmotic pressure of blood (normally, about 30 mm Hg) and capsular pressure (normally, about 15 mm Hg).
- Hence net / effective filtration pressure (EFP) is 10 mm Hg.
- EFP = Hydrostatic Pressure in glomerulus — (Osmotic pressure of blood + Filtrate Hydrostatic pressure) = 55- (30 +15) = 10 mm Hg
- Under the effect of high pressure, the thin walls of the capillary become permeable to major components of blood (except blood cells and macromolecules like protein).
- Thus, plasma except proteins oozes out through wall of capillaries.
- About 600 ml blood passes through each kidney per minute.
- The blood (plasma) flowing through kidney (glomeruli) is filtered as glomerular filtrate, at a rate of 125 ml/min. (180 L/d).
- Glomerular filtrate / deproteinized plasma / primary urine is alkaline, contains urea, amino acids, glucose, pigments, and inorganic ions.
- Glomerular filtrate passes through filtration slits into capsular space and then reaches the proximal convoluted tubule.
Selective reabsorption :
- Selective reabsorption occurs in proximal convoluted tubule (PCT). It is highly coiled so that glomerular filtrate passes through it very slowly. Columnar cells of PCT are provided with microvilli due to which absorptive area increases enormously.
- This makes the process of reabsorption very effective.
- These cells perform active (ATP mediated) and passive (simple diffusion) reabsorption.
- Substances with considerable importance (high threshold) like - glucose, amino acids, vitamin C, Ca++, K+, Na+, Cl are absorbed actively, against the concentration gradient. Low threshold substances like water, sulphates, nitrates, etc., are absorbed passively.
- In this way, about 99% of glomerular filtrate is reabsorbed in PCT and DCT.

Tubular secretion / Augmentation :
- Finally filtrate reaches the distal convoluted tubule via loop of Henle. Peritubular capillaries surround DCT.
- Cells of distal convoluted tubule and collecting tubule actively absorb the wastes like creatinine and ions like
- K+, H+ from peritubular capillaries and secrete them into the lumen of DCT and CT, thereby augmenting the concentration of urine and changing its pH from alkaline to acidic.
- Secretion of Hl ions in DCT and CT is an important homeostatic mechanism for pH regulation of blood.
- Tubular secretion is the only process of excretion in marine bony fishes and desert amphibians.
Distinguish between Selective reabsorption and Tubular secretion:
Selective reabsorption
Tubular secretion
Selective reabsorption is concerned with the selective absorption of useful substances from the glomerular filtrate.
Tubular secretion is transfer of materials from peritubular capillaries to the renal tubular lumen.
Substances with considerable importance (high threshold) like - glucose, amino acids, vitamin C, Ca++, K+, Na+, Cl are absorbed actively, against concentration gradient
In this process, substances like urea, amino acids, glucose, pigments, and inorganic ions are removed from the blood and discharged along with the urine.
Selective reabsorption occurs in Proximal convoluted tubule, Henle’s loop, Distal convoluted tubule and collecting duct.
Tubular secretion occurs in Distal convoluted tubules only.
Concentration of Urine :
Process of concentration of urine (counter current mechanism) :
- Humans can produce concentrated urine in conditions such as low water intake or significant water loss due to sweating. This urine can be four times more concentrated, at 1200 mOsm/L, than blood (300 mOsm/L). As a result, a system known as the countercurrent mechanism operates in the human kidneys.
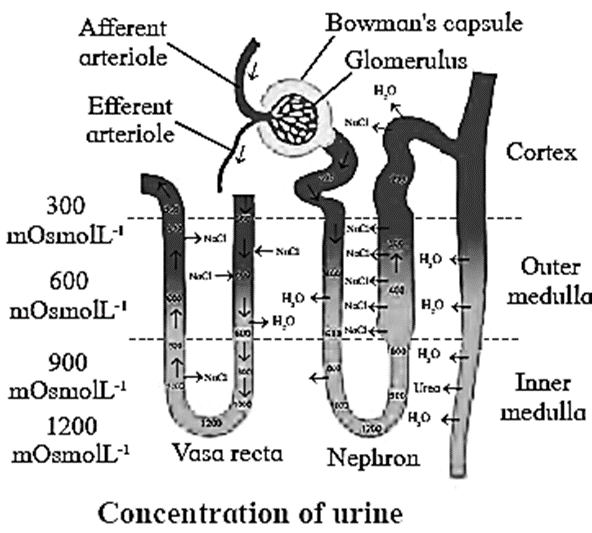
- The countercurrent mechanism operating in the Limbs of Henle’s loop of juxtamedullary nephrons and vasa recta is as follows:
- It involves the passage of fluid from descending to ascending limb of Henle’s loop.
- This mechanism is called countercurrent mechanism, since the flow of tubular fluid is in opposite direction through both limbs.
- In case of the vasa recta, blood flows from ascending to descending parts of itself.
- Wall of descending limb is thin and permeable to water, hence, water diffuses from tubular fluid into tissue fluid due to which, tubular fluid becomes concentrated.
- The ascending limb is thick and impermeable to water. Its cells can reabsorb Na+ and Cl− from tubular fluid and release into tissue fluid.
- Due to this, tissue fluid around descending limb becomes concentrated. This makes more water to move out from descending limb into tissue fluid by osmosis.
- Thus, as tubular fluid passes down through descending limb, its osmolarity (concentration) increases gradually due to water loss and on the other hand, progressively decreases due to Na+ and Cl− secretion as it flows up through ascending limb.
- Whenever retention of water is necessary, the pituitary secretes ADH. ADH makes the cells in the wall of collecting ducts permeable to water.
- Due to this water moves from tubular fluid into tissue fluid, making the urine concentrated.
- Cells in the wall of deep medullar part of collecting ducts are pemieable to urea. As concentrated urine flows through it, urea diffuses from urine into tissue fluid and from tissue fluid into the tubular fluid flowing through thin ascending limb of Henle's loop.
- This urea cannot pass out from tubular fluid while flowing through thick segment of ascending limb, DCT and cortical portion of collecting duct due to impermeability for it in these regions.
- However, while flowing through collecting duct, water reabsorption is operated under the influence of ADH,
- Due to this, urea concentration increases in the tubular fluid and same urea again diffuses into tissue fluid in deep medullar region.
- Thus same urea is transferred between segments of renal tubule and tissue fluid of inner medulla.
- This is called urea recycling; operated for more and more water reabsorption from tubular fluid and thereby excreting small volumes of concentrated urine.
- Osmotic gradient is essential in the renal medulla for water reabsorption by counter current multiplier system.
- This osmotic gradient is maintained by vasa recta by operating counter current exchange system.
- Vasa recta also have descending and ascending limbs. Blood that enters the descending limb of the vasa recta has normal osmolarity of about 300 mOsm/L.
- As it flows down in the region of renal medulla where tissue fluid becomes increasingly concentrated, Na+, Cl− and urea molecules diffuse from tissue fluid into blood and water diffuse from blood into tissue fluid.
- Due to this, blood becomes more concentrated which now flows through ascending part of vasa recta. This part runs through such region of medulla where tissue fluid is less concentrated.
- Due to this, Na+, Cl− and urea molecules diffuse from blood to tissue fluid and water from tissue fluid to blood. This mechanism helps to maintain the osmotic gradient.
Desert mammals, such as camels, have longer Henle loops to reabsorb water to maximum level. As a result, camels excrete concentrated urine.
Composition of Urine :
Composition of normal urine :
Regulation of urine composition :
The composition of urine is determined by the amount of food and liquids consumed by an individual. There are two methods for controlling the composition.
They are as follows:
- Regulating water reabsorption through ADH
- Electrolyte reabsorption though RAAS
(i) Regulating water reabsorption through ADH:
- Hypothalamus in the midbrain has special receptors called osmoreceptors which can detect change in osmolarity (measure of total number of dissolved particles per liter of solution) of blood.
- If osmolarity of blood increases due to water loss from the body (after eating namkeen or due to sweating), osmoreceptors trigger release of Antidiuretic hormone (ADH) from neurohypophysis (posterior pituitary).
- ADH stimulates reabsorption of water from last part of DCT and entire collecting duct by increasing the permeability of cells.
- This leads to reduction in urine volume and decrease in osmolarity of blood.
- Once the osmolarity of blood comes to nonnal, activity of osmoreceptor cells decreases leading to decrease in ADH secretion. This is called negative feedback.
- In case of hemorrhage or severe dehydration too, osmoreceptors stimulate ADH secretion. ADH is important in regulating water balance through kidneys.
- In absence of ADH, diuresis (dilution of urine) takes place and person tends to excrete large amount of dilute urine. This condition called as diabetes insipidus.
(ii) Electrolyte reahsorption through RAAS:
- Another regulatory mechanism is RAAS (Renin Angiotensin Aldosterone System) by Juxta Glomemlar Apparatus (JGA).
- Whenever blood supply (due to change in blood pressure or blood volume) to afferent arteriole decreases (e.g. low BP/dehydration), JGA cells release Renin. Renin converts angiotensinogen secreted by hepatocytes in liver to Angiotensin I. ‘Angiotcnsin converting enzyme’ further modifies Angiotensin I to Angiotensin II, the active form of hormone. It stimulates adrenal cortex to release another hormone called aldosterone that stimulates DCT and collecting ducts to reabsorb more Na+ and water, thereby increasing blood volume and pressure.
(iii) Atrial natriuretic peptide (ANP):
- Action of ADH and RAAS leads to increase in blood volume and osmolarity.
- A large increase in blood volume and pressure stimulates atrial wall to produce atrial natriuretic peptide (ANP). ANP inhibits Na+ and Cl− reabsorption from collecting ducts inhibits release of renin, reduces aldosterone and ADH release too.
- This leads to a condition called Natriuresis (increased excretion of Na+ in urine) and diuresis.
Function of Angiotensin II :
- It constricts arterioles in kidney thereby reducing blood flow and increasing blood pressure.
- It stimulates PCT cells to enhance reabsorption of Na+, Cl− and water.
- It stimulates adrenal cortex to release another hormone called aldosterone that stimulates DCT and collecting ducts to reabsorb more Na+ and water, thereby increasing blood volume and pressure.
Q. Which hormones and factors are involved in regulation of kidney function?
Ans. Hormones like ADH, Renin, Angiotensin and Atrial Natriuretic Peptide (ANP) are involved in regulation of kidney function.
Remember : Kidneys participate in synthesis of calcitriol, the active form of Vitamin D which is needed for absorption of dietary calcium. Deficiency of calcitriol can lead to brittle bones.
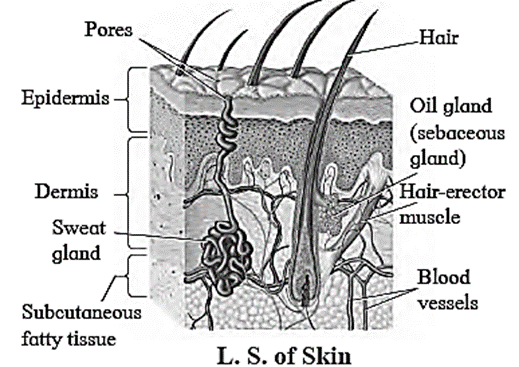
Role of Other Organs in Excretion : Various organs other than the kidney participate in excretion. They are as follows: Skin: The skin of many organisms is thin and permeable. It helps in diffusion of waste products like ammonia. Human skin however is thick and impermeable. It shows presence of two types of glands namely, sweat glands and sebaceous glands. Lungs :
Disorders and Diseases :
- Presence of excessive albumin in urine (albuminuria) indicates injury to endothelialcapsular membrane as a result of increased blood pressure, injury or irritation of kidney cells by substances such as toxins or heavy metals.
- Excessive ketone body levels in urine can be induced by diabetes, malnutrition, or a low carbohydrate diet.
- The presence of leucocytes in urine indicates the risk of kidney or other urinary organ infection.
Some disorders and diseases related to the excretory system are as follows
- Kidney stones
- Uremia
- Nephritis
- Renal Failure
- Ketonuria
- Albuminaria
Kidney stones :
Kidney stones are also called renal calculi. They may be formed in any portion of urinary tract, from kidney tubules to external opening.
Urolithiasis is the process of formation of stones in the kidney, bladder and/or urethra.
Types of Kidney stones:
Depending on their composition, kidney stones are classified into the following types.
- Calcium stones : These are usually calcium oxalate or calcium phosphate stones.
- Struvite stones : These are formed in response to bacterial infection caused by urea-splitting bacteria.
- They grow in size quickly and become quite large.
- Uric acid stones : These stones usually affect people drinking less water or consuming high protein diet.
- Cystine stones : It is a genetic disorder that causes the kidney to excrete too much of certain amino acid.
Symptoms:
- Intermittent pain below rib cage in back and side ways. Hazy, brownish / reddish / pinkish urine. Frequent urge to pass urine. Pain during micturition.
Diagnosis:
- Uric acid content of blood, colour of urine, kidney X-ray, sonography of kidney are different diagnostic tests prescribed depending on symptoms.
Uremia :
The normal content of urea in blood is 0.01 to 0.03 %. If the level of urea in blood rises above 0.05%, the condition is known as uremia. It may lead to kidney failure.
Nephritis :
- Nephritis is kidney inflammation characterised by proteinuria
- It is produced by increased permeability of the glomerular capsule membrane, allowing significant amounts of proteins to escape from the blood into the urine.
- This caused a change in blood colloidal osmotic pressure, which caused fluid to flow from the blood to the interstitial spaces.
- It appears as edoema.
Renal failure :
Renal failure is the decrease or cessation of glomerular filtration and is classified into two types.
Acute Renal failure (ARF):
- ARF is sudden worsening of renal function that most commonly happens after severe bleeding.
- There is a decrease in urine output (0ligouria/ scanty urine i.e., less than 400 ml/day or less than 0.5 ml/kg/h in children).
- Other causes of ARF may include acute obstruction of both ureters or nephrotoxic drugs.
- ARF can be detected biochemically by elevated serum creatinine levels.
Chronic kidney disease (CKD) :
- It is the progressive and generally irreversible decline in glomerular filtration rate (GFR).
- It may be caused due to chronic glomerulonephritis.
- It can be detected by reduced kidney size and possibility of anaemia.
Haemodialysis : When renal function of a person falls below 5-7 %, accumulation of harmful substances in blood begins. In such a condition, the person has to go for artificial means of filtration of blood i.e. haemodialysis. Process of haemodialysis : Drawbacks of haemodialysis :

Peritoneal dialysis :
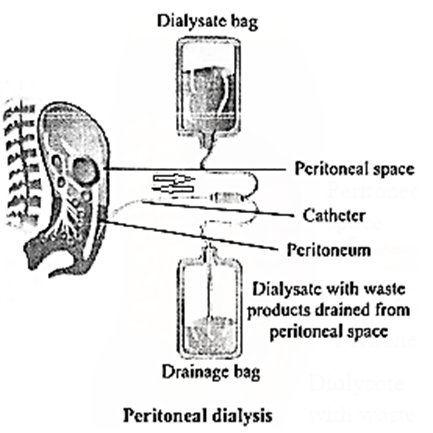
Remember : Dialysis is regarded as a 'holding measure' until a renal transplant can be performed or sometimes as the only supportive measure in those for whom a transplant would be inappropriate.
Kidney transplant :
- It is organ transplant of a healthy kidney into a patient with end stage renal disease. Kidney transplantation is classified as cadaveric (deceased donor) or living donor kidney transplant.
- Living donor kidney transplant are further classified as genetically related (living-related) or non-related (living non-related) transplants.
Precaution taken in kidney transplant :
- The recipient's immune cells may reject the foreign kidney by mounting an immunological response against it.
- Immunosuppressive medications suppress the immune system, lowering the possibility of transplant rejection.
- As a result, immunosuppressants are given to a person having kidney transplant.
Restrictions on diet for kidney patients: Excessive water consumption. Reduce your intake of foods high in oxalate, such as soy products, rhubarb, beets, okra, spinach, Swiss chard, sweet potatoes, almonds, and tea. Eat a diet low in animal protein and salt. Reduce your calcium supplement intake (if you take any), but make sure you get enough calcium from your diet.
Main Page : – Maharashtra Board Class 11th-Biology – All chapters notes, solutions, videos, test, pdf.
Previous Chapter : Chapter-14- Human Nutrition – Online Notes
Next Chapter : Chapter-16-Skeleton and Movement – Online Notes
We reply to valid query.