|
Topics to be Learn : Part-1
- Reproduction
- Asexual Reproduction in animals
- Sexual Reproduction in animals
- Menstrual cycle (Ovarian cycle)
- Gametogenesis
Topics to be Learn : Part-2
- Fertilization / Syngamy
- Embryonic development
- Pregnancyl Gestation
- Placenta
- Parturition
- Lactation
- Reproductive Health
- Birth control
- Sexually Transmitted Diseases (STDs)
- Infertility
|
Reproduction : Reproduction is defined as the biological process of formation of new life forms from pre-existing similar life.
- Through reproduction, species can survive over a long period.
- Reproduction in animals occur mainly by two methods, i.e. asexual and sexual.
Asexual Reproduction in animals :
Common and primitive method among animals.
Meiosis or the gamete formation and fertilization process does not take place in asexual reproduction.
Single parent is involved and offspring identical to parent. Also called clone.
- E.g. Gemmule formation and budding.
Gemmule formation :
Gemmule formation :

- Gemmule is an internal bud formed only in sponges. In sponges, during unfavourable conditions this method of asexual reproduction is adopted.
- Gemmule is thus an asexually produced mass or aggregation of dormant archeocytes cells. They develop into a new organism.
- Around archaeocytes, amoebocytes secrete a layer of thick resistant membrane.
- Gemmules hatch and develop into new individual when favourable conditions return.
- Example: Spongilla.
[collapse]
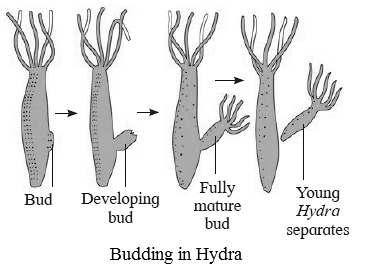
Budding :
Budding : Ii is a simple method of asexual reproduction seen in coelenterates (Hydra and corals) and in some colonial ascidians.
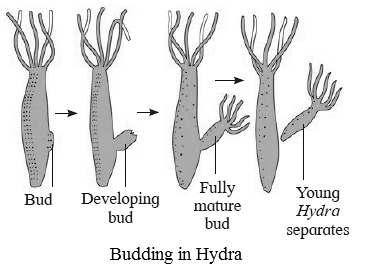
- A bud, i.e. small outgrowth is produced towards the basal end of the body, in Hydra.
- Bud develops as a bud which grows and forms tentacles and develops (get transformed) into a new individual.
- .This young Hydra later detaches from parent and becomes a separate organism.
[collapse]
Sexual Reproduction in animals :
- Offspring is produced by fusion of gametes or amphimixes in sexual reproduction. For the formation of gametes, both male and female parent undergo meiosis in their gonads.
- Two main phases in the life of sexually reproducing animals : Juvenile phase/pro-reproductive phase which involves growth and reproductive/maturity phase in which sex organs undergo maturation.
- Animals are either seasonal breeders like goat, sheep and donkey which breed only in particular season or continuous breeders like human and apes who can breed throughout the year.
Human reproduction :
Sequential steps in the process of human reproduction : gametogenesis, insemination, internal fertilization, zygote formation and embryogenesis, gestation and parturition followed by lactation.
Primary Sex organs — testes (testis : singular)in male and ovaries (ovary : singular) in female. ‘
Secondary or accessory Sex organs – Organs other than testis in male and Organs other than ovaries in female.
Secondary sexual characters in males — Presence of beard, moustache, hair on the chest, muscular body, enlarged larynx (Adam’s apple), etc.
Secondary sexual characters in females -Developed breast, broader pelvis, high pitched voice. etc.
Sexual dimorphism : The phenomena by which sexes can be identified externally.
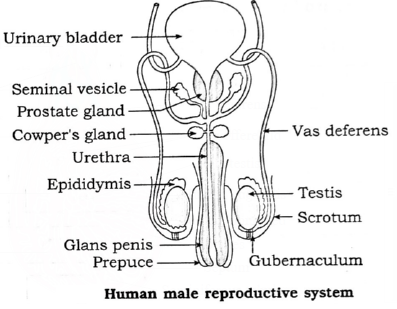
Male Reproductive System :
Male Reproduction System : Parts of male reproductive system - Testes, accessory ducts, glands and external genitalia.
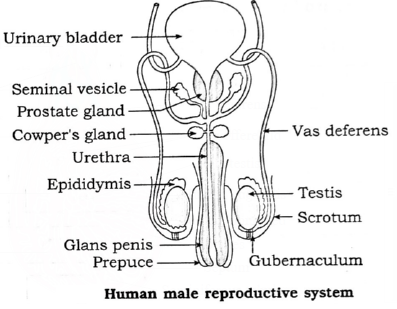
Testes - A pair of testes, mesodermal in origin, are formed in the lower abdominal cavity
- Position : They are located in a pouch called scrotum. During early foetal life, the testes develop in abdominal cavity and later they descend into the scrotal sac.
- Structure : Testes are male gonads with dimensions ofabout 4.5. cm length, 2.5 cm Width and 3 cm thickness. There are about 200 to 300 lobules in each testis in which there are seminiferous tubules that form rete testis.
- Functions : Testes produce sperms and secrete male sex hormone, androgen or testosterone.
Accessory ducts : Rete testis, vasa efferentia, epididymis, vas deferens, ejaculatory duct and urethra together form the accessory ducts of male reproductive system.
Rete testis :
- Position : Towards posterior side of testis
- Structure : Formed by convergence of Seminiferous tubules
- Functions : Carry sperms to vasa efferentia
Vasa efferentia :
- Position : They arise from rete testis and end into the epididymis.
- Structure : Vasa efferentia are 12-20 fine tubules.
- Functions :The sperms from the testis are carried by these ducts to the epididymis.
Epididymis :
- Position : They are located on the posterior border of each testis.
- Structure : Epididymis are long and coiled tubes having three parts, viz. caput, corpus and cauda epididymis.
- Functions : The sperms undergo maturation in epididymis.
Vasa deferentia :
- Position :Each vas deferens enters the abdominal cavity through the inguinal canal and then ascends in the form of spermatic cord.
- Structure : Vasa deferentia are a pair of 40 cm long tubular structures that arise from cauda epididymis.Vas deferens of each side is joined by the duct from seminal vesicle to form ejaculatory duct.
- Function : Carry Sperms from epididymis to ejaculatory ducts.
Ejaculatory duct :
- Position : About 2 cm long pair of ducts formed by joining vas deferess and the ducts of seminal vesicles
- Structure : Tube like structure, 2 cm long pass through prostate gland and open into the urethra.
- Functions :Seminal fluid containing spermatozoa are carried by ejaculatory duct to the urethra.
Urethra :
- Position : Long tube extends through the Penis.
- Structure :About 18-20 cm long tube. Open outside by urethral orifice or urethral meatus.
- Functions : The male urethra provides a common passage for the urine and semen hence is also called urinogenital duct.
Accessory glands : Associated with male reproductive system are : (a) Seminal vesicles (b) Prostate gland and (c) Cowper’s or Bulbourethral glands.
Every accessory gland has secretion which helps in functions of reproductive system.
Seminal vesicles :
- Position : On the posterior side of urinary Bladder
- Structure : Pair of small fibromuscular glands
- Functions : Secretion of seminal vesicles contains fructose, fibrinogen and prostaglandins. Fructose provides energy for sperm movement. Fibrinogen coagulates the semen into bolus. Prostaglandin aids in faster movement of sperms towards the ovum in female body. Contributes about 60% of the total volume of semen.
Prostate gland :
- Position : Underneath the urinary bladder
- Structure : Large and single gland made up of 20-30 lobes..Surrounds the urethra
- Functions : Secretion is White and slightly acidic, prostatic fluid. Forms about 30 % of volume of semen. Contains citric acid, acid phosphatase and enzymes. Acid phosphatase protects the sperms from acidic environment of vagina.
Cowper’s or Bulbourethral glands :
- Position : On either side of urethra.
- Structure : Small, pea sized and paired glands.
- Functions : Secretion of alkaline, viscous mucous like fluid. Acts as lubricant during copulation.
Extenal genitalia : External genitalia consists of penis and scrotum.
Penis :
- Position : In pubic region in front of Scrotum.
- Structure : It is cylindrical, erectile and pendulous organ through which passes the urethra. It contains three columns of erectile tissues which has abundant blood sinuses. The tip is called glans penis while the retractible fold of skin on penis is called prepuce.
- Functions : Penis is the copulatory organ used for insemination or deposition of sperms in female genital tract.
Scrotum :
- Position : Lower abdomen, behind the penis
- Structure :The scrotum is a pouch of pigmented skin arising from lower abdominal wall. It protects testes within it.
- Functions : Scrotum acts as thermoregulator. Testis are suspended in scrotum by spermatic cord.
Terms associated with external genitalia of male.
- Inguinal canal : The passage through which testes descend into scrotum.
- Gubernaculum : Fibro-muscular band present in the scrotum.
- Cryptorchidism : Failure of testis to descend into scrotum which may cause sterility.
- Three bundles of erectile tissues in penis: (i) Paired Corpora cavernosa. (ii) Median corpus spongiosum.
Semen : Single ejaculate of semen is 2.5 to 4.00 ml of viscous. alkaline and milky fluid (pH 7.2 to 7.7) containing 400 million sperms and secretions of epididymis, prostate gland, and Cowper’s glands. It is rich in fructose, Ca++, bicarbonates and prostaglandins.
[collapse]
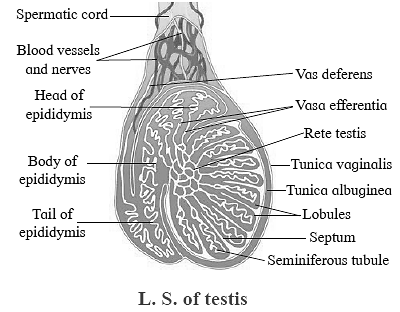
Histology of testis :
- External coverings of testis seen in L.S. from outer to inner side tunica vaginalis, tunica albuginea and tunica vasculosa.
- Testicular mass divided into 200-300 testicular lobules by tunica albuginea.
- Each lobule has 1-4 seminiferous tubules.
- In between the seminiferous tubules there are interstitial cells of Leydig or Leydig's cells.
- They secrete the male hormone androgen or testosterone.
- Internal lining of cuboidal germinal epithelial cells or spermatogonia inside the seminiferous tubules.
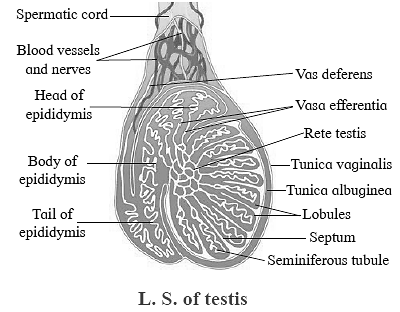
- Few large pyramidal cells called Sertoli or sub-tentacular cells (nurse cells) Sertoli cells provide nutrition to the developing sperms.
- Various stages of developing sperms such as spermatogonia, primary spermatocyte, secondary spermatocyte, spermatids and sperms are seen in the seminiferous tubules.
Female Reproductive System :
Female Reproductive System : The female reproductive system consists of the following parts :

- A pair of ovaries
- A pair of fallopian tubes. (Also called oviducts, but usually this term is used for lower animals)
- Uterus
- Vagina
- External genitalia (vulva)
- A pair of vestibular glands
- A pair of mammary glands
Ovaries :
- Ovaries are situated in the abdomen in upper lateral part of the pelvis near the kidneys. Their dimensions are about 3 cm in length, 1.5 cm in breadth and 1.0 cm thick. They are solid, oval or almond shaped organs.
- Ovaries produce ova and they are also endocrine in nature as they produce estrogen, progesterone, relaxin, activin and inhibin.
- Ovarian hormones bring about secondary sexual characters. They also control menstrual cycle, pregnancy and parturition.
Fallopian tubes/oviducts :
Fallopian tubes lie horizontally over peritoneal cavity. These are about 10 to 12 cm long, narrow, muscular structure lined by ciliated epithelium.
They transport the ovum after ovulation from the ovary to the uterus.
Fallopian tube can be subdivided into the following three parts :
- The infundibulum which bears a number of finger-like processes called fimbria at its free border.
- Infundibulum is funnel-shaped having ostium which receives ova released from the ovary. .
- The second part is the ampulla where the fertilization takes place.
- The last part is short cornua or isthmus which opens into the uterus.
Uterus/Womb :
Uterus is a pear-shaped, highly muscular thick walled, hollow organ measuring about
8 cm in length, 5 cm in width and 2 cm in thickness.
Uterus has the following three parts : Fundus, Body or corpus and Cervix.
The cervix communicates above with the body of the uterus by an aperture, the internal os and with vagina below by an opening the external os.
Uterus has three-layered wall. These layers are:
- Perimetrium : An outer serous layer.
- Myometrium : The middle thick muscular layer of smooth muscles.
- Endometrium : The inner highly vascular mucosa that has many uterine glands.
Uterus receives the ovum from fallopian tube. It develops placenta during pregnancy for the nourishment of foetus. At the time of parturition, it expels the young one at birth.
Vagina :
- Vagina is a highly distensible fibro-muscular tube that lies between the cervix and the vestibule.
- It is about 7 to 9 cm in length and is internally lined by stratified and non-keratinised epithelium. The vaginal wall has inner mucous lining.
- Vagina acts as a birth canal as well as copulatory passage. It also allows passage of menstrual flow.
- Vagina opens into vestibule by vaginal orifice which may be covered with hymen which is also a mucous membrane.
External genitalia or vulva or pudendum : The external genitalia consists of five parts; viz. labia majora, labia minora, mons veneris, clitoris and vestibule.
A pair of vestibular glands/Bartholin’s glands: These glands open into the vestibule and release a lubricating fluid.
A pair of mammary glands / breasts : These are the accessory organs of female reproductive system for production and release of milk after parturition.
[collapse]
Puberty / Sexual maturity in Females :
Puberty is achieved due to gonadotropins such as FSH and LH secreted by the anterior pituitary. These hormones stimulate the ovaries. The ovaries in turn produce estrogen and progesterone, which brings about secondary sexual characters in female. Thus she attains the puberty.
Reproductive age of female : The period from menarche to menopause.
The beginning of menstrual cycle or menarche takes place due to these hormonal changes at about 10 to 14 years of age.
But the women do not remain reproductively active after the age of 50 due to hormonal imbalance. This is called menopause or cessation of reproductive cycles.
Absence of enough gonadotropins and unresponsive ovarian cells cause menopause at 45 to 50 years of age.
Structure and development of the ovary: The process of oogenesis starts in ovary much before the birth of the female baby. The various developing follicles and their fate is shown in the following flow chart :
Histological structure of ovary : :
Histological structure of ovary :
- Each ovary is a compact structure differentiated into a central part called medulla and the outer part called cortex.
- The cortex is covered externally by a layer of germinal epithelium while the medulla contains the stroma or loose connective tissue with blood vessels, lymph vessels and nerve fibres.
- Different stages of developing ovarian follicles are seen in the cortex. Each primordial follicle has at its centre a large primary oocyte (2n) surrounded by a single layer of flat follicular cells, then gradually it matures.
- In the ovary during each menstrual cycle there is a maturation of primordial follicles into multilayered primary, secondary and Graafian follicles.
- Every Graafian follicle has three layers, viz. theca externa, theca interna and membrane granulosa which are from outer to inner side. A space called antrum filled with liquor folliculi is present inside the follicle.
- There is a small hillock of cells called cumulus oophours or discus proligerus over which the ovum is lodged. The ovum in turn is covered by vitelline membrane, zona pellucida and corona radiata from inner side to outer surface.
- Ovarian cortex also shows corpus luteum, or yellow body formed from empty Graafian follicle after ovulation. Corpus luteum is converted into corpus albicans or white body in case of absence of conception.
[collapse]
Menstrual cycle (Ovarian cycle) : Menstrual cycle involves a series of cyclic, changes in the ovary and uterus. The cyclic events are regulated by gonadotropins from pituitary and the hormones from ovary.
The cyclic events in woman are repeated within approximately 28 days.
Menstrual cycle is divided into following phases, viz.
Phases of menstrual cycle and their hormonal control : :
Menstrual phase (Day 1-5) :
- Menstrual phase occurs in the absence of fertilization.
- During menstruation, uterine endometrium is sloughed off. Level of progesterone and estrogen decrease during this phase resulting into release of prostaglandins which cause this rupture.
- Blood about 45-100 ml, tissue fluid, mucus, endometrial lining and unfertilized oocyte and other cellular debris is discharged through vagina as a menstrual flow. The endometrial lining becomes about 1 mm thin.
- Fibrinolysin does not allow blood to clot during this period.
- Pituitary starts secreting FSH, which further makes many primordial follicles to develop into primary and few of them into secondary follicles.
Follicular phase (Day 5-14) : Follicular phase in ovary that coincides with proliferative phase in uterus. / Post menstrual phase:
- During this phase in the ovary the follicles develop while in uterus the endometrium starts proliferating. 6 to 12 secondary follicles start developing but usually only one of them becomes Graafian follicle due to action of FSH.
- Developing secondary follicles secrete the hormone estrogen.
- Estrogen brings about regeneration of endometrium. Further proliferation of endometrium causes formation of endothelial cells, endometrial or uterine glands and network of blood vessels.
- Endometrium’s thickness becomes 3-5 mm.
Ovulatory phase (Day 14-15) :
- Ovulation occurs in this phase. Mature Graafian follicle ruptures and secondary oocyte is released into the pelvic region of abdomen.
- Ovulation occurs due to surging quantity of LH from pituitary.
Luteal phase (Day 16 to 28) : Luteal phase in ovary which coincides with secretory phase in uterus.
- Since the empty Graafian follicle converts itself into corpus luteum under the influence of LH, this phase is called luteal phase in ovary. At the same time, the uterine endometrium thickens and becomes more secretory and hence it is called secretory phase in uterus.
- Corpus luteum secretes progesterone, some amount of estrogens and inhibin. These hormones stimulate the growth of endometrial glands which later start uterine secretions.
- Endometrium becomes more vascularized becomes 8—1O mm. in thickness. These changes are the preparation for the implantation of the ovum if fertilization occurs.
- In absence of fertilization, corpus luteum can survive for only two weeks and then degenerate into a non-secretory white scar called corpus albicans.
- If ovum is fertilized, woman becomes pregnant and hormone hCG (human
- Chorionic Gonadotropin) is secreted by chorionic membrane of embryo which keeps corpus luteum active till the formation of placenta.
- If the ovum is fertilized corpus luteum is retained.
- A once embryo gets implanted in the endometrium. it starts secretion of human ---chorionic gonadotropin (hCG) which extends the life of corpus luteum.
- Presence of hCG in maternal blood and urine is an indicator of pregnancy
- If ovum is not fertilized, corpus luteum regresses and forms corpus albicans. Then the next menstrual Cycle begins.
[collapse]
Gametogenesis : The process of formation of gametes in sexually reproducing animals is called gametogenesis.
- Sperm is the male gamete and ovum/(Egg is the female gamete.
- The gametes are formed from primordial germ cells of gonads.
- Spermatogenesis : The process by which sperms are formed is called spermatogenesis.
- In the testis, i.e. male gonads there are seminiferous tubules which are lined by germinal epithelium.
- Cells of germinal epithelium undergo spermatogenesis and form sperms.
- In between the germinal cells there are nurse cells or cells of Sertoli which provide nourishment to the developing sperms.
Phases of spermatogenesis :
Phases of spermatogenesis : There are three phases of spermatogenesis, viz. multiplication phase, growth phase and maturation phase.
Germinal cells are called primordial germ cells

- Multiplication phase : Repeated mitotic divisions produce large number of spermatogonia which are diploid (2n).
- Growth phase : The spermatogonium accumulates food and grows in size. This is now called primary spermatocyte.
- Maturation phase : The primary spermatocyte undergoes first meiotic division. At the end of this division two haploid secondary spermatocytes are formed. Secondary spermatocyte undergoes second meiotic division and produce spermatid.
Spermatids are non-motile and non-functional.
They undergo metamorphosis in the process of spermiogenesis and mature into motile sperms. Each haploid spermatogonium thus forms four haploid spermatids which later transform into the sperms.
[collapse]
Changes occurring during spermiogenesis :
- Increase in sperm length
- Distinction of centrioles into proximal and distal one.
- Formation of axial filament from distal centriole
- Formation of spirally coiled mitochondria.
- Formation of acrosome from Golgi complex.
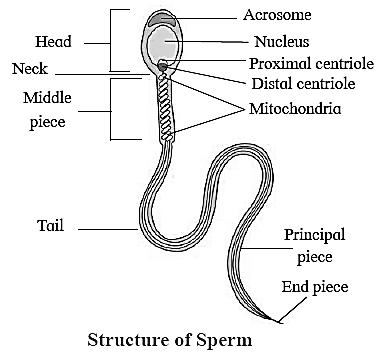
Structure of the sperm (spermatozoa) :
Structure of the sperm (spermatozoa) :
- Microscopic, elongated haploid motile male gamete measuring about 0.055 mm [60p] in length.
- Produced by the process of spennatogenesis.
- Their viability remains viable for seventy-two hours, but can fertilize the ovum in first 12 to 14 hours only.
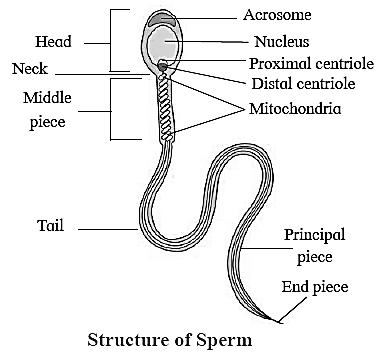
Parts of sperm : The sperm consists of head, neck, middle piece and tail.
Head :
- Head is the main part which is flat and oval and has a large nucleus and an acrosome.
- Acrosome is formed from Golgi complex. It secretes enzyme hyaluronidase which helps in penetration of the egg during fertilization.
- The acrosome and anterior half of nucleus is covered by a fibrillar sheath.
Neck : Neck is short region having two centrioles.
- The proximal centriole plays a role in first cleavage of zygote.
- The axial filament of the sperm is formed by the distal centriole.
Middle piece :
- Middle piece acts as a power house for sperm.
- It bears many spirally coiled mitochondria or Nebenkern around the axial filament.
- The mitochondria supply energy for the sperm to swim in the female genital tract with a speed of about 1.5 to 3 mm per minute.
- Posterior half of nucleus, neck and middle piece of sperm are covered by a sheath.
Tail :
- The tail is formed of cytoplasm and is long, slender and tapering structure.
- The axial filament is a fine thread-like structure that arises from the distal centriole and traverses the middle piece and tail.
- Nine accessory fibres are present surrounding the two central longitudinal axial filaments. ‘
- Tail lashes and helps the spermatozoa to swim.
[collapse]
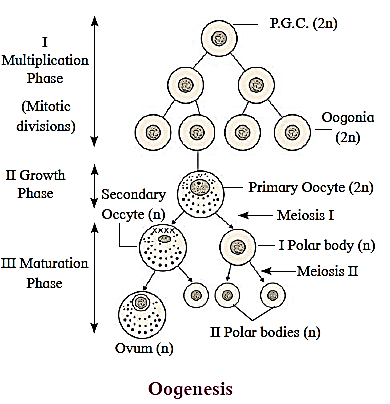
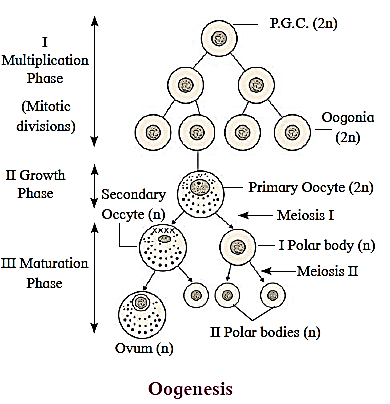
Oogenesis : Oogenesis takes place in ovary by which the secondary oocyte is formed.
Phases of oogenesis :
Phases of oogenesis :
- Phase of multiplication : In the phase of multiplication, large number of oogonia are formed.
- Phase of growth : In the phase of growth, one of the oogonia becomes large. It is now called primary oocyte.
- Phase of maturation : In this phase the primary oocyte undergoes meiosis—I and forms large haploid secondary oocyte.
- There is equal nuclear division but unequal cytoplasmic division during the phase of maturation. Secondary oocyte and polar bodies undergo arrested meiotic-I division. Secondaly oocyte completes the meiosis-II if and only if it undergoes fertilization.
[collapse]
Structure of ovum (secondary oocyte) :
Structure of ovum (secondary oocyte) :
- The ovum discharged by the ovary during ovulation is actually a secondary oocyte.
- Rounded, haploid, non-motile. Female gamete is largest cell of the body.
- Measures about 0.1 mm or 100m in diameter.
- It is microlecithal, i.e. almost free of yolk.
- It has abundant cytoplasm or ooplasm having a large eccentric nucleus surrounded by vitelline membrane.
- Centriole is absent in the ovum.
- Ovum shows polarity having two poles.
- Animal pole is the side which shows the presence of polar body and nucleus while the opposite side is termed as vegetal pole.
- The ovum is enclosed by two additional coats inner, thin, transparent and noncellular zona pellucida and outer, thick cellular corona radiata.
- Between the vitelline membrane and zona pellucida there is a narrow perivitelline space.
- The zona pellucida is secreted by ovum itself While corona radiata is formed of radially elongated follicular cells which are glued together by hyaluronlc acid.

[collapse]
Next Part ->>




Thanks sir
Discus proligerus and cumulus oophorus have not been explained correctly..
Please do the needful..
Noted and forwarded to the concerned.
If necessary, it will be updated.
Thanks for your valuable suggestion.